The aorta is the largest artery of the human body. It begins from the heart, runs through the chest and abdomen and at the level of the navel splits into two branches, the iliac arteries. The part within the chest is called thoracic aorta. In some patients the thoracic aorta is weak and dilates like a balloon creating a thoracic aortic aneurysm.
The main risk is rupture which can be fatal due to internal bleeding. Less commonly peripheral embolization can occur. In most aneurysms there is a significant amount of clot (thrombus) within the aorta. In some cases a piece of clot can travel and block any blood vessel of the abdomen or lower extremity (peripheral embolization).

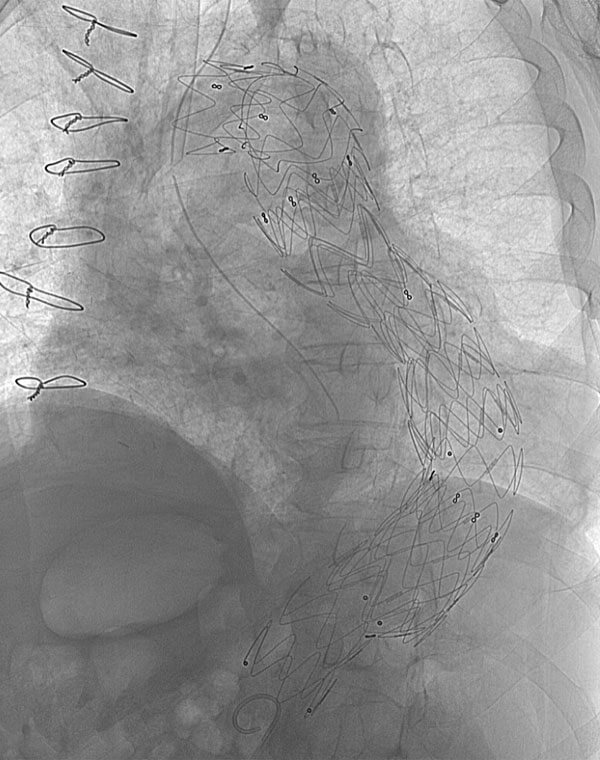
Percutaneous Thoracic Endograft
Percutaneous Thoracic Endograft
Thoracic aortic aneurysm is more common in men, older than 60 years. Fortunately, if diagnosed early (before rupture), treatment is simple and effective. Most patients do not have any symptoms. Some may feel chest or back pain, hoarseness, cough or shortness of breath. Sudden chest or lower back pain or loss of consciousness suggests rupture. On rare occasions patients may feel pain in the abdomen or lower extremity due to peripheral embolization.
The etiology of the aneurysm is unknown. Risk factor include age >60y, 1st degree relative with an aneurysm, high blood pressure and smoking. Diagnosis is confirmed with CT or MRI scan. A thoracic aneurysm can be suspected by a chest x ray or cardiac Duplex Ultrasound.
The risk of rupture is relative to the diameter. If it is smaller than 5,5cm, patients should monitor the aneurysm with CT or MRI, control their blood pressure and stop smoking.
Repair of the aneurysm is required when it becomes larger than 5,5cm, when there is a significant increase of diameter or when it becomes symptomatic.
There are two methods of treatment, minimally invasive (endovascular) and open surgical repair.
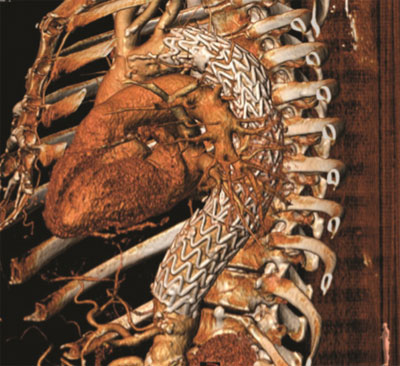
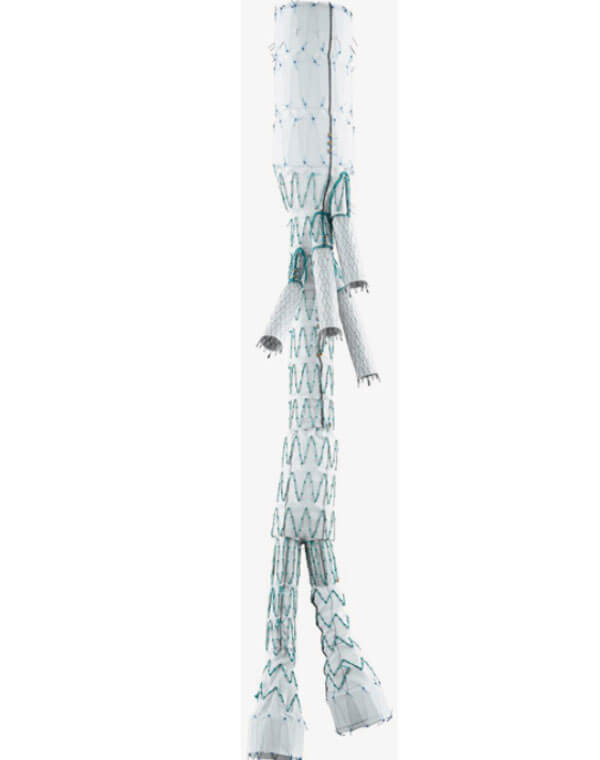
Endovascular Repair of Thoracic Aneurysm
During the minimally invasive procedure the repair of the aneurysm is performed from within the vessel (this is why it is called endovascular). Under local anesthesia, the vascular surgeons puncture the femoral arteries of the leg and then place an endograft within the thoracic aorta. The patient is discharged in 1 – 2 days, there is no postoperative pain and recovery is very fast.
Open surgical repair requires general anesthesia and an incision of the chest and abdomen. The aorta is replaced with a synthetic graft. Usually after the operation, the patient is transferred to ICU for 1 – 2 days and he is discharged after 7 – 10 days. Full recovery requires 3 months.
The advantages of the minimally invasive procedure are obvious: no general anesthesia, no abdominal incision, no postoperative pain, early discharge and early recovery. The endovascular repair is performed in most but not all patients.
For both methods there are indications and contradictions.
The results of the endovascular repair are excellent when:
a) It is performed by experienced vascular surgeons in patients suitable for this technique.
b) It is performed in state of the art hybrid operating rooms which combine the safety of the operating room with the superb imaging capabilities of the angiography suite.
c) Last generation endovascular devices are used.
Patients with thoracic aortic aneurysm should consult vascular surgeons with experience in both endovascular and open surgical repairs in order to receive the most appropriate method of treatment.
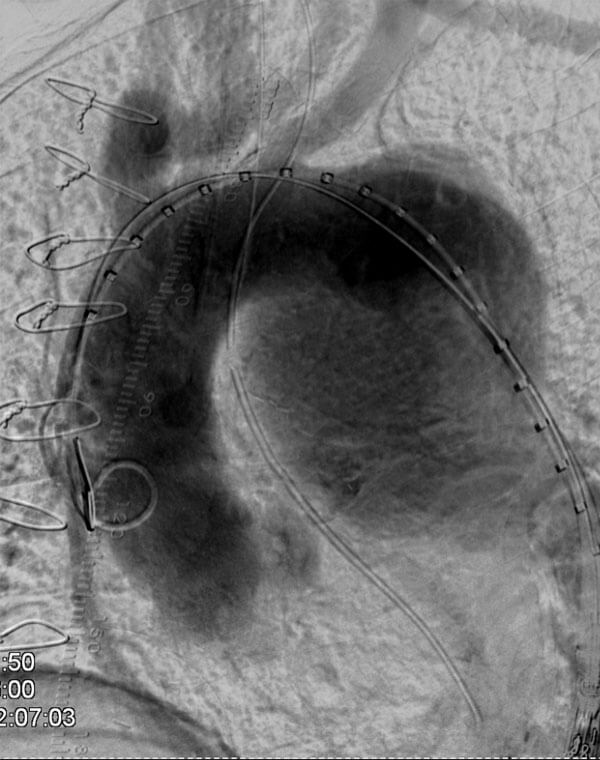

Endovascular Repair of Thoracic Aneurysm