Splachnic arteries supply blood to the internal organs of the entire body.
The arteries are normally smooth and unobstructed on the inside. In some cases, a sticky substance called plaque (atherosclerosis) builds up in the wall of the arteries. Risk factors are age, family history, high cholesterol, diabetes, high blood pressure, obesity and smoking.
The most important arteries that develop atherosclerosis are the renal arteries (please refer to “renal artery disease”) and the ones of the digestive tract called celiac, superior mesenteric and inferior mesenteric artery.
Symptoms in patients with stenosis of the arteries of the digestive tract usually develop when in there is involvement of at least two of them. The most common ones ate pain after eating and loss of weight. In severe life-threatening cases necrosis of the small or large intestine may develop.
Diagnosis of splachnic artery disease of the digestive tract is confirmed easily by Duplex Ultrasound. In some cases, CT Angiography, MR Angiography or Digital Angiography is needed to document the diagnosis.
Treatment is needed in selected patients with involvement of at least two of the three arteries and depends on symptoms and severity of narrowing. Besides medical therapy, invasive treatment is performed with two methods. The first one is minimally invasive (angioplasty with stent). The second one is open surgical procedure.
Currently, most patients with splachnic artery disease can be treated with minimally invasive procedures. During minimally invasive procedures, the repair of the artery is performed from within the vessel (endovascular repair). Under local anesthesia, the vascular surgeon punctures the artery of the leg or arm and uses a special balloon to open the vessel. In many cases a small metal tube (stent) is used to keep the artery open. The following day, the patient is discharged from the hospital and recovery is immediate without any pain.
Open surgical procedures (bypass) require general anesthesia and long abdominal incision. A detour around the blockage is created using synthetic graft or one of the patient’s own vein.
The advantages of the minimally invasive procedure are obvious: no general anesthesia, no abdominal incision, no postoperative pain, early discharge and early recovery. The endovascular repair is performed in most but not all patients.
For both methods there are indications and contradictions.
The results of the endovascular repair are excellent when:
a) It is performed by experienced vascular surgeons in patients suitable for this technique.
b) It is performed in state-of-the-art hybrid operating rooms which combine the safety of the operating room with the superb imaging capabilities of the angiography suite.
c) Last generation endovascular devices are used.
Patients with splachnic artery disease of the digestive tract should consult vascular surgeons with experience in both endovascular and open surgical repairs in order to receive the most appropriate method of treatment.
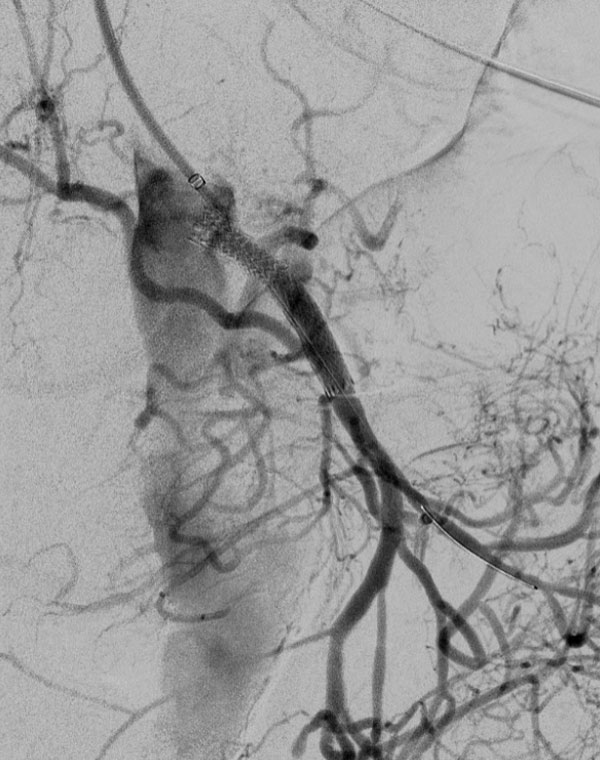
In the following pictures you can see patients from our clinic with successful endovascular repair of celiac, superior and inferior mesenteric artery.

Celiac artery stenosis

Celiac artery stent

Superior mesenteric artery stenosis
Superior mesenteric artery stent

Inferior mesenteric artery stenosis

Inferior mesenteric artery stent